Understanding Glaucoma
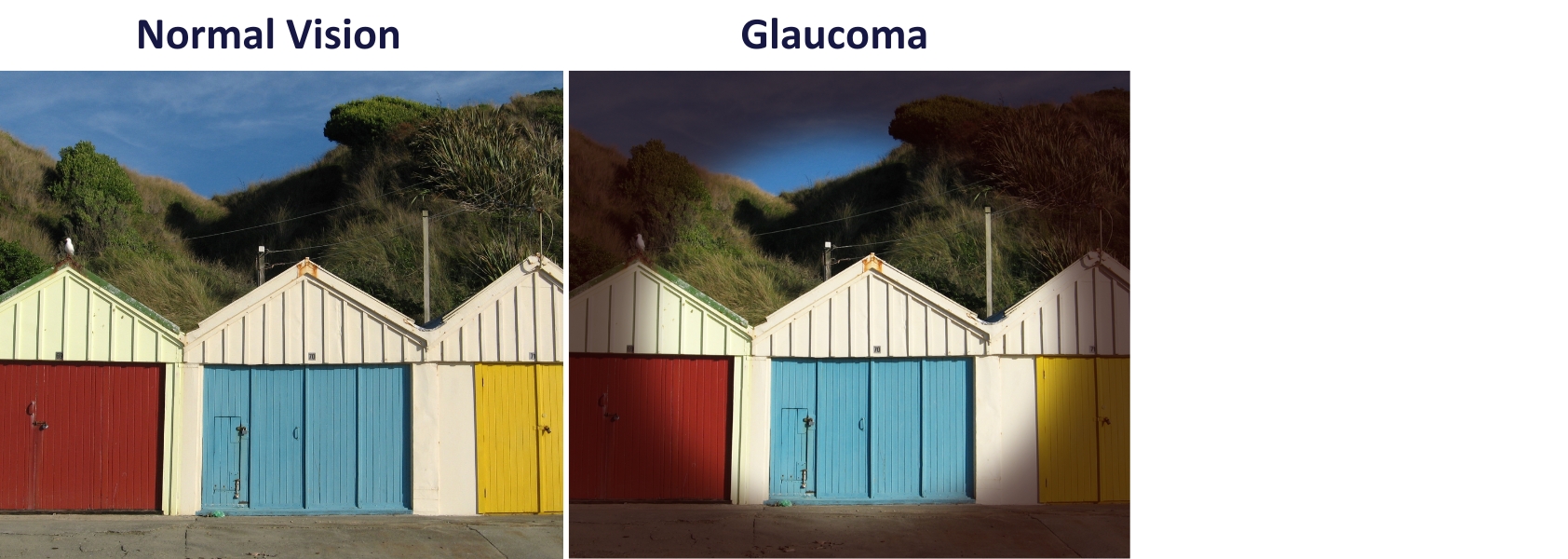
Glaucoma is a progressive condition that affects the optic nerve. Nerve fibres that connect the retina to the brain die off and fail to regenerate, eventually affecting vision. In New Zealand, glaucoma is the second most common cause of blindness.
Glaucoma can happen at any age, but it’s most common in people over 60. If you have symptoms, risk factors or a family history of glaucoma, talk to your Auckland Eye ophthalmologist sooner rather than later.
Risk factors
There’s no single cause of glaucoma, but there are some factors that can elevate your risk.
These include:
Age – screen every five years after age 40, and every two years after 60.
Family history of glaucoma
Previous eye injuries
High or low blood pressure
A range of conditions including diabetes, sleep apnoea, migraines and high myopia (near-sightedness)
Types of glaucoma
Primary open-angle glaucoma
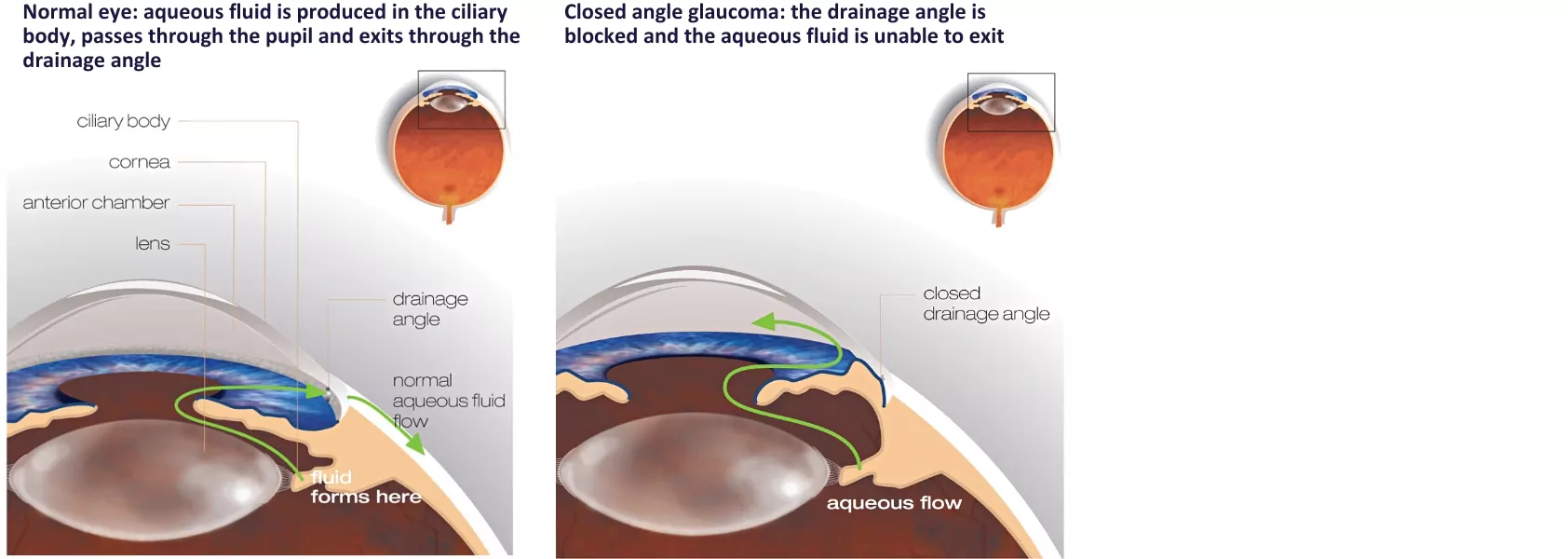
This common type of glaucoma occurs when the drainage function of the eye is not working properly, increasing fluid pressure on the optic nerve. It can develop slowly without apparent symptoms.
Normal-tension glaucoma
In this form of glaucoma, optic nerve damage occurs when eye pressure is within a normal range – usually because of other factors or health conditions. It is more common in people of Asian descent, people with migraines and those with circulatory issues.
Angle-closure glaucoma
In this uncommon, serious form of glaucoma, a blockage in the eye’s drainage system causes sudden IOP. Sufferers will usually feel sudden, severe pain or aching in the eye, along with redness, blurred vision and coloured rings around lights. Nausea and vomiting are also common. Vision can be impacted quickly, so seek emergency treatment if you experience these symptoms.
Secondary glaucoma
Other eye problems, including trauma, inflammation and blocked blood vessels, can cause glaucoma.
Congenital and juvenile glaucoma
In rare cases, glaucoma can appear in babies, children and young adults. In babies under a year old, this is known as congenital glaucoma. Signs include light sensitivity, watery eyes and cloudy-looking corneas. In older children and adolescents, the condition is called juvenile glaucoma, with symptoms such as redness around the eyes, light sensitivity, loss of vision, head or eye pain and excessive blinking or rubbing of the eyes. If you notice these symptoms, seek immediate advice from a specialist.
Treating glaucoma: reducing pressure, stabilising symptoms
There is no cure for glaucoma. However, if it’s caught early, treatment can slow or prevent further loss of vision.
Non-surgical treatments
Eye drops and medication
If your glaucoma is diagnosed during the early stages, eye drops will probably be the first treatment. You may also be prescribed oral medication to either slow the rate of aqueous fluid production or improve drainage.
Selective laser trabeculoplasty (SLT) – for primary open-angle glaucoma
SLT is a non-invasive treatment that targets the drainage ducts of the eye. The tissue in the area reacts to the heat generated by the laser, and drainage of fluids improves, lowering the IOP for one to five years.

Surgical treatments
Incisional surgery
This common technique involves creating a channel or hole through the wall of the eyeball (the sclera), allowing excess aqueous fluid to drain from the eye slowly. Although the surgery is safe, the opening may heal over, meaning further surgeries or other treatments are necessary.
Micro-invasive glaucoma surgery (MIGS)
Micro-invasive glaucoma surgery is suitable for people with mild to moderate glaucoma. The procedure involves placing tiny tubes or stents into specific parts of the eye to improve drainage of aqueous fluid.
Drainage tube placement
Drainage tube devices may be inserted if other glaucoma treatments have been ineffective. These tiny devices are placed under the eye’s surface layer and connected to a curved filtering plate that sits on the outside of the eye. Fluid drains through the tube onto the plate, where the body absorbs it. In most cases, you won’t be able to see or feel the device in your eye.
Recovery after glaucoma surgery
Most glaucoma surgery doesn’t require a general anaesthetic. After resting for an hour or two after the procedure, you will usually be able to leave – but you will need someone to drive you home. Don’t drive for at least 24 hours after surgery.
Your eye will need around two weeks to heal and recover from surgery. During this time, avoid possible infection or damage – for example, swimming, strenuous exercise and handling soil during gardening.
Your surgeon will follow up with you in the days after your surgery to check your results.











